What are cataracts?
Cataracts are a very common condition – they’re the main cause of vision impairment worldwide and affect approximately 2.5 million people aged 65 and up in England and Wales alone.
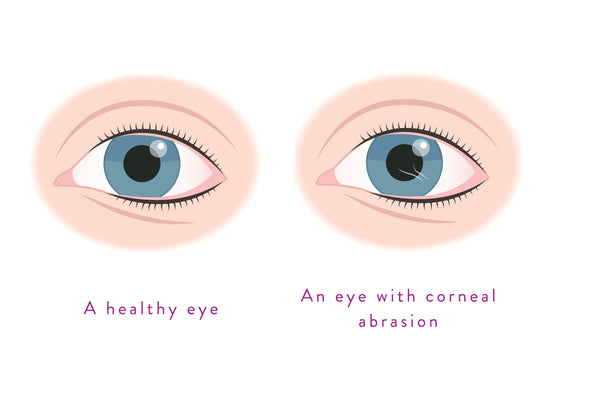
Cataracts occur when part of your eye lens (the part of your eye that focuses light) goes cloudy. It usually starts off as small patches but can grow overtime. They can affect one or both eyes and can range from a slight cloudiness to total vision loss.
Types of cataracts
Most cataracts are age-related – they happen because of normal changes in your eyes as you get older. But cataracts can develop for other reasons such as after an eye injury or after surgery for another eye problem like glaucoma. There are many types of cataracts but there are 3 main types that are most commonly seen in patients.
- Nuclear cataracts – affects the centre of the lens
- Cortical cataracts – affects the outer edge of the lens
- Posterior subcapsular cataracts – affects the back of the lens
The different types of cataracts affect different areas of the lens, however it is not always distinguishable to the person with cataracts which area is affected.
If you notice dark or cloudy spots in your vision, it’s best to visit your optometrist to have them examine your eyes in case it is cataracts.
Symptoms
Cataracts develop slowly over time and, because they’re not painful or cause soreness or irritation, many people don’t notice symptoms at first. They tend to affect both eyes but each eye can be affected differently.
Cataract symptoms include:
- Blurred, misty, or cloudy vision
- Bright lights that are dazzling or uncomfortable to look at
- Faded colours or colours have a brown or yellow tinge to them
- Difficulty seeing in either dim or very bright light
- You may see halos around bright lights such as headlights
- Spots or patches in your vision that are unclear.
Early signs of cataracts

The first symptoms you might experience with cataracts are blurry vision, faded colours, and more difficulty seeing in the dark than normal. Squinting doesn’t help to clear the cloudiness.
These symptoms can also be caused by other eye conditions so if you’re experiencing a sudden onset of any of the symptoms we’ve listed, make an appointment with your optometrist to have your eyes examined.
Causes
In general, cataracts are a natural part of ageing. When we are young (assuming you don’t need glasses) we can focus clearly at a distance and change our focus to see things clearly up close. This is achieved through the alteration of the shape of the crystalline lens (a small m&m sized structure that sits behind the iris). When you’re young, due to the cellular structure and density, our lens changes shape when we want to focus.
But as we age, the lens produces more cells to maintain its structure and, because it is not able to slough away the old cells as our skin does, our eye lenses become more dense and rigid. Because of this, the lens can not change shape the way it used to to focus. This is called presbyopia.
Cataracts are a natural continuation of normal ageing of our eyes, often developing after you reach around 65 years of age. Unlike our skin, the old cells in your eyes can not slough away – instead, they build up and cause clouding of the vision. Around half of people aged 80 will either have cataracts or have had surgery to correct them.
There are other contributing factors that can accelerate the development of cataracts:
- Lifelong exposure to UV light
- Smoking
- A poor diet lacking in vitamins
- Long-term use of steroidal medications
- Certain health conditions, such as diabetes
- A family history of cataracts
- Regularly drinking excessive amounts of alcohol
Cataracts and myopia

Myopia is the medical term for being short-sighted – you have trouble focusing on items far away.
Cataracts can relate to myopia in two different ways. One, if you have normal vision and develop cataracts, you can become slightly myopic. Two, if you are already highly myopic and have been for a long time, you are more likely to develop cataracts and other eye diseases.
Diagnosis
Cataracts can be picked up with normal eye tests. On occasion, your optometrist may opt for a dilated eye exam to view the cataract in more detail. These exams are simple and straightforward – you will be given some eye drops to dilate your pupil. Then your optometrist will check your eyes for cataracts and other eye problems. For this test it is recommended that you wear sunglasses afterwards as you will be more sensitive to light for a few hours.
Those who are more prone to developing them early or those over 60 should get check ups as recommended by their eye specialist, ideally at least every 2 years to keep track of any problems.
Treatment
The only treatment proven to be effective at removing cataracts is surgery. However, despite it being low risk (1/1,000 complications) there is still some risk involved which needs to be considered.
Until that point, the best way of managing your cataracts in the early stages is to ensure you have an up-to-date prescription for your glasses or contact lenses.
You can also make other small adjustments to make life easier such as:
- Using brighter lights at home or work
- Wear anti-glare sunglasses
- Wear sunglasses when outside in sunny weather as there is evidence that UV exposure can accelerate the process of cataract formation
Cataracts surgery
Surgery is the only treatment that is proven to be effective for cataracts. A number of experimental eye drops to treat cataracts have been trialled with limited results, therefore most patients with cataracts go on to require surgery. The usual surgery performed to remove cataracts is called phacoemulsification.

Even if your cataracts are mild, they will eventually need surgery. Cataract surgery involves removing the affected lens (by a process known as phacoemulsification) and replacing it with a new, artificial lens (also called an intraocular lens, or IOL). This surgery is considered very safe and very few patients report complications post-surgery.
Takeaway
Cataracts are extremely common and occur in around half of all adults over the age of 65. They happen due to a natural part of your eyes ageing. They can be worrisome and impact your daily life but can be easily treated thanks to a successful surgery.
Therefore, it is important to have regular check ups with your optometrist, especially if you are over the age of 65 or are more prone to developing them such as having a family history, have diabetes, or if you’re a heavy smoker or drinker.